Which anticoagulation is safe in renal failure?
Unfractionated heparin (UFH) is preferred because it has a short half‐life that allows for the anticoagulant effect to wear off within 1 to 4 hours, even in patients with severe renal dysfunction at high hemorrhagic risk.
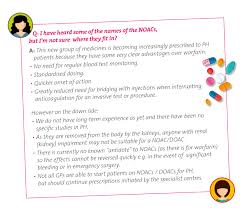
What are the new oral anticoagulants in CKD?
In the general population, newer oral anticoagulants (dabigatran, rivaroxaban, apixaban, and edoxaban) reduce risk of stroke or systemic embolism and bleeding versus warfarin in patients with AF, and they are increasingly prescribed in patients with CKD and patients with ESKD.
What is the newest medication for kidney disease?
and INDIANAPOLIS, September 22, 2023 – The U.S. Food and Drug Administration (FDA) has approved Jardiance® (empagliflozin) 10 mg tablets to reduce the risk of sustained decline in estimated glomerular filtration rate (eGFR), end-stage kidney disease, cardiovascular death and hospitalization in adults with chronic …
What are NOACs for kidney disease?
In routine clinical practice, NOACs were used less frequently than warfarin in patients with reduced kidney function. NOACs were consistently associated with similar or better effectiveness and safety than warfarin in patients with different degrees of kidney impairment.
What is the DOAC of choice for renal failure?
Apixaban and rivaroxaban are the two DOACs that have been used the most in patients with advanced CKD (CrCl of <30 mL/min). Also, these are the only two DOACs with FDA approval for patients undergoing hemodialysis.
Is apixaban safe in renal failure?
Apixaban clearance is less dependent on renal function compared to other direct‐acting oral anticoagulants. Data from retrospective studies suggest that apixaban has at least similar efficacy in stroke prevention for NVAF, but lower bleeding risk compared to VKA in dialysis cohorts [5, 6].
What are NOACs new oral anticoagulants?
New oral anticoagulants (NOACs) are an alternative for vitamin K antagonists (VKAs) to prevent stroke in patients with non-valvular atrial fibrillation (AF). Unlike VKAs, these anticoagulants do not require routine INR monitoring and possess favorable pharmacological properties.
Is LMWH safe in renal failure?
Patients with renal failure thus are potentially at risk for bleeding as a result of impaired LMWH clearance and prolonged anticoagulant effects. Observational studies report increased bleeding using LMWH in patients with renal insufficiency compared with those without renal impairment (3).
Is Xarelto safe in renal failure?
When analyzed by dose, dialysis patients prescribed the full dose of XARELTO 20 mg (which is not recommended in this patient population11) had a higher risk of major bleeding than patients who were prescribed the lower dose of XARELTO 15 mg (which is the recommended dose for patients with renal impairment11).
What is the latest treatment for chronic kidney disease in the UK?
The National Institute for Health and Care Excellence (NICE), has issued draft guidance recommending a new treatment for patients with chronic kidney disease (CKD) called empagliflozin, which has been shown to slow down progression to kidney failure and reduce the risk of heart attacks and strokes.
What are the latest advances in kidney disease treatment and research?
These developments include FDA approvals for: A drug to slow down the decline of eGFR in people with kidney disease. A phosphate absorption inhibitor drug. The first fully-FDA-approved treatment for a rare kidney disease called IgA nephropathy.
Which anticoagulation is best for kidney failure?
Warfarin. Warfarin remains a popular choice for many patients with CKD, especially for those with ESKD, despite having a narrow therapeutic range and a susceptibility to multiple drug and food interactions. Patients with CKD often require lower daily doses to achieve therapeutic levels due to downregulation of CYP450.
Which anticoagulant is used in CKD patients?
Warfarin has long been the anticoagulant of choice for the prevention of stroke in patients with AF and CKD.
Is edoxaban safe in renal failure?
Edoxaban is cleared through the kidney regardless of renal function. The FDA issued a warning on taking edoxaban for patients with CrCl > 95 mL/min because of a reported decrease in efficacy for the prevention of systemic embolism compared with warfarin [7].
Which NOACs are best for CKD patients?
The preferred agents are the NOACs apixaban and rivaroxaban, levels of which are only modestly affected by kidney disease. Both medications have proven efficacy and safety against warfarin in moderate kidney disease.
Can dabigatran be used in renal failure?
Dabigatran is mainly eliminated by renal excretion, and hence it is contraindicated in patients with creatinine clearance (CrCl) of <30 mL/min [1]. Dabigatran increases the risk for bleeding, particularly in acute kidney injury (AKI) [2].
Is Eliquis better than Xarelto for kidney disease?
Eliquis may be the better choice if you have kidney problems. If you have trouble remembering to take your medications, a DOAC that you can take once a day (like Xarelto) may be a better option than a DOAC that’s taken twice a day (like Eliquis). Only Xarelto is FDA approved for certain uses in children.
Is DOAC safe in renal failure?
No DOAC is licensed for use below a creatinine clearance of 15 ml/min. Patients below this renal function (including those on dialysis) must not be started on a DOAC or if on one will need to be changed to an alternative anticoagulant. 2.
Is dalteparin safe in renal failure?
These differences may be explained by the fact that smaller LMWH chains (enoxaparin) are cleared primarily by the kidneys, whereas larger chains (dalteparin, tinzaparin) have greater clearance by nonrenal mechanisms. Thus, dalteparin and tinzaparin may be preferred in patients with renal impairment.
What blood thinners are good for kidney patients?
New blood thinners, so-called DOAK, could be an attractive alternative to the traditional substance warfarin, even in advanced kidney disease or dialysis treatment, according to a thesis. It focuses on this patient group and investigates whether blood-thinning drugs protect against stroke due to blood clots.
What are the newer anticoagulants?
Newer anticoagulants, novel oral anticoagulants (NOAC) or directly acting oral anticoagulants (DOAC) include a direct thrombin inhibitor (dabigatran) and factor Xa inhibitors (rivaroxaban, apixaban, and edoxaban). These medications work differently than warfarin while still achieving similar anticoagulation effects.
What are the three new oral anticoagulants?
Until recently, vitamin K antagonists, such as warfarin, were the only available oral anticoagulants. This situation changed with the recent introduction of the non-vitamin K antagonist oral anticoagulants (NOACs), which include dabi- gatran, rivaroxaban, apixaban, and edoxaban.
What is the safest anticoagulant in renal failure?
Apixaban may be a safer and more effective option for the treatment of VTE in dialysis patients compared to warfarin, although this systematic review highlights the need for further studies in patients taking anticoagulation for VTE treatment or VTE prophylaxis in patients with advanced CKD (CrCl < 30 ml/min) to …
Is fondaparinux safe in renal failure?
Introduction. The literature recommends against the use of fondaparinux in patients with kidney failure and dialysis as it may, with repeated dosing, accumulate and put patients at risk of bleeding.
Is enoxaparin safe in renal failure?
Enoxaparin bioaccumulates and causes bleeding if it is administered in therapeutic doses without dose adjustment to patients with impaired renal function. Bioaccumulation appears to be greatest in patients with a creatinine clearance of less than 30 ml/min and when therapeutic LMWH doses are used.
What blood thinners are good for kidney patients?
New blood thinners, so-called DOAK, could be an attractive alternative to the traditional substance warfarin, even in advanced kidney disease or dialysis treatment, according to a thesis. It focuses on this patient group and investigates whether blood-thinning drugs protect against stroke due to blood clots.
Is LMWH safe in renal failure?
Patients with renal failure thus are potentially at risk for bleeding as a result of impaired LMWH clearance and prolonged anticoagulant effects. Observational studies report increased bleeding using LMWH in patients with renal insufficiency compared with those without renal impairment (3).
Is fondaparinux safe in renal failure?
Introduction. The literature recommends against the use of fondaparinux in patients with kidney failure and dialysis as it may, with repeated dosing, accumulate and put patients at risk of bleeding.
Is Eliquis or Xarelto better for kidneys?
Eliquis may be the better choice if you have kidney problems. If you have trouble remembering to take your medications, a DOAC that you can take once a day (like Xarelto) may be a better option than a DOAC that’s taken twice a day (like Eliquis). Only Xarelto is FDA approved for certain uses in children.
Are novel oral anticoagulants effective in patients with AF and CKD?
Can anticoagulant prescribing be used in chronic kidney disease (CKD)?
Do patients with chronic kidney disease receive anticoagulation or antiplatelet therapy?
What are the most common anticoagulant scenarios in kidney patients?
So, what’s the deal with newer anticoagulants? They are basically a newer generation of blood thinners that work in a different way than the older ones. They’re designed to be more targeted, have fewer side effects, and are easier to use.
The Challenge: Anticoagulation in Renal Failure
Before we dive into the specifics, let’s talk about the challenges of anticoagulation in renal failure. People with kidney disease have a tough time getting rid of waste products through their kidneys. This means that many medications, including anticoagulants, can build up in their system and cause problems.
The Old Guard: Warfarin
We used to rely heavily on warfarin, but it’s a bit of a pain to use. You need regular blood tests to monitor how well it’s working, and the dose has to be adjusted based on your diet and any other medications you’re taking.
Plus, warfarin is notorious for interacting with a whole bunch of other meds. This can be tricky for folks with kidney disease, who are often on a cocktail of medications.
The New Kids on the Block: Direct Oral Anticoagulants (DOACs)
This is where the direct oral anticoagulants (DOACs) come in. These are a newer class of medications that work by directly blocking the activity of certain clotting factors in your blood.
They are considered *safer and more convenient* than warfarin because:
They are easier to use. They usually don’t require frequent blood tests, and the dose is pretty consistent.
They have fewer interactions with other drugs. This is a big deal for people with kidney disease who are taking a bunch of other medications.
They are often more effective.
Types of DOACs
There are several types of DOACs available, and each one has its own quirks:
1. Factor Xa Inhibitors
Rivaroxaban (Xarelto)
Apixaban (Eliquis)
Edoxaban (Savaysa)
These medications work by blocking Factor Xa, a key clotting factor in your blood.
2. Direct Thrombin Inhibitors
Dabigatran (Pradaxa)
This medication directly inhibits thrombin, the final enzyme in the clotting cascade.
DOACs in Renal Failure: A Closer Look
Now, let’s talk about how DOACs are used in people with renal failure. The good news is that many DOACs are actually *safer and easier to use* in this population.
However, it’s important to remember that renal failure can affect how these drugs are metabolized and excreted from the body.
Kidney Function Matters!
Here’s the deal:
Mild to moderate renal impairment: In most cases, DOACs can be used with caution, but *dose adjustments may be needed*.
Severe renal impairment: Some DOACs may not be as effective or might be dangerous in people with severe renal impairment. This is why it’s *essential to talk to your doctor* about your specific situation.
Choosing the Right DOAC
Your doctor will consider a bunch of factors when choosing the right DOAC for you, including:
Severity of your kidney disease
Type of blood clot you have
Other medications you’re taking
Your personal risk factors for bleeding
Safety First: Potential Side Effects
Like any medication, DOACs can have side effects, and bleeding is the most common one.
It’s crucial to be aware of the warning signs of bleeding and to contact your doctor right away if you experience any of the following:
Unusual bruising or bleeding
Blood in your urine or stool
Nosebleeds that won’t stop
Unexplained headaches or dizziness
FAQs
What if I miss a dose of my DOAC?
This is something you should always talk to your doctor about. They can tell you the best way to handle missed doses based on your specific medication.
How long will I need to take my DOAC?
It depends on your individual situation. Your doctor will help you determine how long you need to take your medication.
Can I take a DOAC if I have a history of bleeding problems?
DOACs may not be right for everyone with a history of bleeding problems. It’s essential to have a conversation with your doctor about your specific situation.
Can I drink alcohol while taking a DOAC?
This is a question for your doctor. Alcohol can interact with certain medications, and it’s crucial to get their guidance.
Is there a way to reverse the effects of a DOAC?
Yes, there are medications available to reverse the effects of DOACs in case of excessive bleeding.
What other medications can interact with DOACs?
There are a number of medications that can interact with DOACs, so it’s important to tell your doctor about all the medications you are taking, including over-the-counter drugs and supplements.
The Bottom Line
Newer anticoagulants, especially direct oral anticoagulants (DOACs), have revolutionized the treatment of blood clots, especially for people with kidney disease.
These medications can be *safer and more convenient* than traditional warfarin, but it’s important to work closely with your doctor to ensure you are taking the right medication and dose.
Remember, every individual is different, so there’s no one-size-fits-all answer when it comes to anticoagulation. Be sure to discuss your specific situation with your doctor to get the best possible treatment.
See more here: What Are The New Oral Anticoagulants In Ckd? | Newer Anticoagulants In Renal Failure
Anticoagulation in chronic kidney disease: from guidelines to
Based on the available data, this review outlines the benefit‐risk ratio of all types of anticoagulants in each stage of CKD and provides practical recommendations for accurate dosage adjustment, reversal of antithrombotic effect, and monitoring of renal National Center for Biotechnology Information
Anticoagulant strategies for the patient with chronic kidney disease
Chronic kidney disease (CKD) is a global health problem affecting up to 14% of the adult population in developed countries. On the basis of current guidelines, patients with CKD will often fulfil criteria for both short-term and long-term anticoagulation. National Center for Biotechnology Information
Use of Newer Anticoagulants in Patients With Chronic Kidney
Conclusion: Newer anticoagulants should be used with caution in patients with mild-to-moderate renal impairment. Unfractionated heparin remains the preferred anticoagulant in most… Medscape
Antithrombotic Therapy in Patients With Chronic
End-stage renal disease is a US administrative definition that includes patients treated by dialysis or transplantation regardless of the GFR level. Many calculators are available to estimate the GFR. The AHA/ASA Journals
Newer Oral Anticoagulant in Chronic Kidney Disease: What we
All of the NOACs are dependent on renal clearance to some degree and so the risk of NOAC associated bleeding may be expected to be greater in patients with renal failure. Apixaban may be at least as safe as (or possibly safer than) warfarin in PubMed
Use of newer anticoagulants in patients with chronic kidney
Newer anticoagulants should be used with caution in patients with mild-to-moderate renal impairment. Unfractionated heparin remains the preferred anticoagulant in most patients with severe renal impairment even though its use is associated with Oxford Academic
Use of Newer Anticoagulants in Patients With Chronic Kidney
Use of Newer Anticoagulants in Patients With Chronic Kidney Disease. Bob L. Lobo. Disclosures. Am J Health Syst Pharm. 2007;64 (19):2017-2026. 0. Drug Dosing Considerations in… Medscape
Use of newer anticoagulants in patients with chronic kidney disease
Newer anticoagulants should be used with caution in patients with mild-to-moderate renal impairment. Unfractionated heparin remains the preferred anticoagulant in most patients with severe renal impairment even though its use is associated with PubMed
UK prescribing practice of anticoagulants in patients with chronic …
A survey to gain insight into anticoagulant prescribing practice in the setting of chronic kidney disease (CKD) across the UK was disseminated via renal and haematology networks. Areas of anticoagulant use included patients with venous BMC Nephrology
See more new information: pilgrimjournalist.com
New Anticoagulants In Renal Patients: Practical Aspects. Prof. Hamza Kabil
Anticoagulation And Renal Failure – Case Study
New Anticoagulants In Renal Patients Practical Aspects
When Renal Disease Worsens, Anticoagulation Still Lowers Stroke Risk
The New Anticoagulants In Cardiovascular Disease: Atrial Fibrillation And Beyond
Link to this article: newer anticoagulants in renal failure.
See more articles in the same category here: https://pilgrimjournalist.com/wiki/